Gynaecological and Maternity Health: A Comprehensive Guide
- Dr Prajakta S Shinde

- Oct 12, 2025
- 5 min read
Updated: Dec 19, 2025
Gynaecological and maternity health is vital for women's overall well-being. Being aware of common conditions that affect this area can empower women to seek timely medical advice and treatment. In this blog post, I will explore prevalent gynaecological and maternity conditions, their symptoms, and treatment options.
Understanding Gynaecological Conditions
Peri-Pubertal Issues
Peri-pubertal issues in young girls encompass a range of physical, emotional, and social challenges as they transition into adolescence. This critical developmental phase typically occurs between ages 9 and 14. It is marked by the onset of menstruation and significant hormonal changes.
During this time, girls may experience various physical changes, including breast development, growth spurts, and the onset of menstruation. These changes can lead to body image concerns and anxiety. Emotionally, they may face mood swings and heightened sensitivity due to fluctuating hormone levels. Additionally, social pressures, such as the desire for acceptance among peers and the influence of media portrayals of femininity, can exacerbate feelings of insecurity.
Parents and caregivers play a vital role in providing support and education during this time. They help young girls navigate these challenges with confidence and resilience.
Infertility: Understanding the Causes
Infertility, defined as the failure to conceive, can arise from various causes, attributed to either male or female factors. In women, common causes include hormonal imbalances, ovulatory disorders, age-related decline in fertility, and structural issues such as blocked fallopian tubes or uterine abnormalities.
In men, infertility may result from low sperm count, poor sperm motility, or structural problems in the reproductive system. Lifestyle factors such as obesity, smoking, excessive alcohol consumption, and environmental toxins can also contribute to infertility in both genders.
Management of infertility often involves a comprehensive approach. This includes lifestyle modifications, medical treatments such as hormone therapy or medications to induce ovulation, and assisted reproductive technologies like in vitro fertilization (IVF). Additionally, addressing underlying health conditions and providing psychological support can play a crucial role in the overall management of infertility.
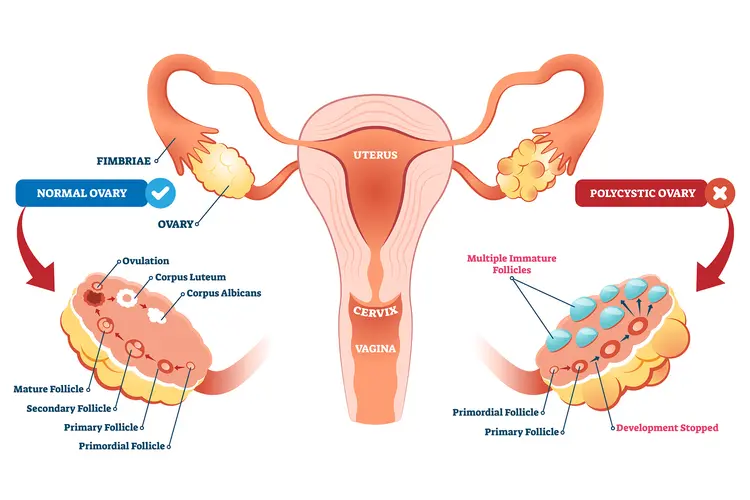
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder affecting about 1 in 10 women of reproductive age. Key symptoms include irregular menstrual cycles, excessive hair growth (hirsutism), acne, and obesity. Women may also have multiple cysts on their ovaries, which can be detected during an ultrasound.
Effective treatment for PCOS often begins with lifestyle changes, such as a balanced diet and regular exercise. Studies have shown that losing just 5-10% of body weight can significantly improve symptoms. Additionally, hormonal contraceptives are commonly prescribed to regulate menstrual cycles and address symptoms like acne and hair growth.
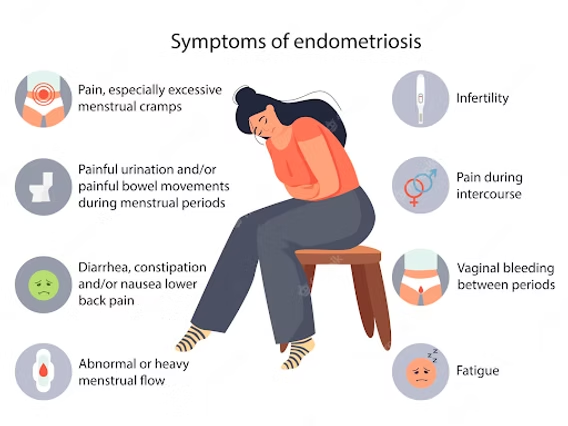
Endometriosis: A Painful Condition
Endometriosis affects approximately 10% of women worldwide. This condition arises when tissue similar to the lining of the uterus grows outside of the uterus. It leads to pain during menstruation, heavy periods, and sometimes infertility.
Treatment options for endometriosis vary based on severity. Over-the-counter pain relievers can help manage pain. Hormonal therapies, including birth control pills, may help reduce or eliminate menstruation. For severe cases, surgical options like laparoscopy can remove endometrial tissue, offering relief for about 70% of women after surgery.
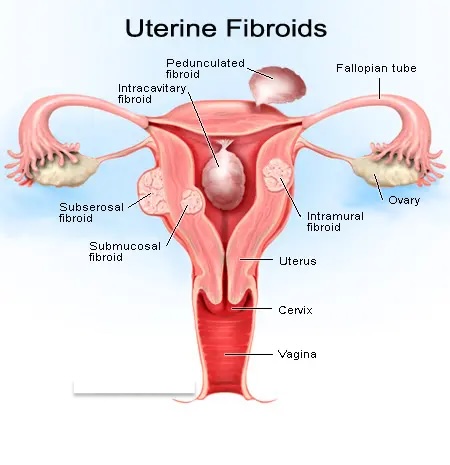
Uterine Fibroids: Common Yet Manageable
Uterine fibroids are non-cancerous growths in the uterus that occur in about 20-50% of women by age 50. Many women with fibroids experience no symptoms, while others report heavy menstrual bleeding, pelvic pain, and frequent urination.
Treatment options include regular monitoring if symptoms are mild, medications like hormonal therapy to manage bleeding, and surgical options such as myomectomy or hysterectomy. About 30% of women with symptomatic fibroids may ultimately require surgery.
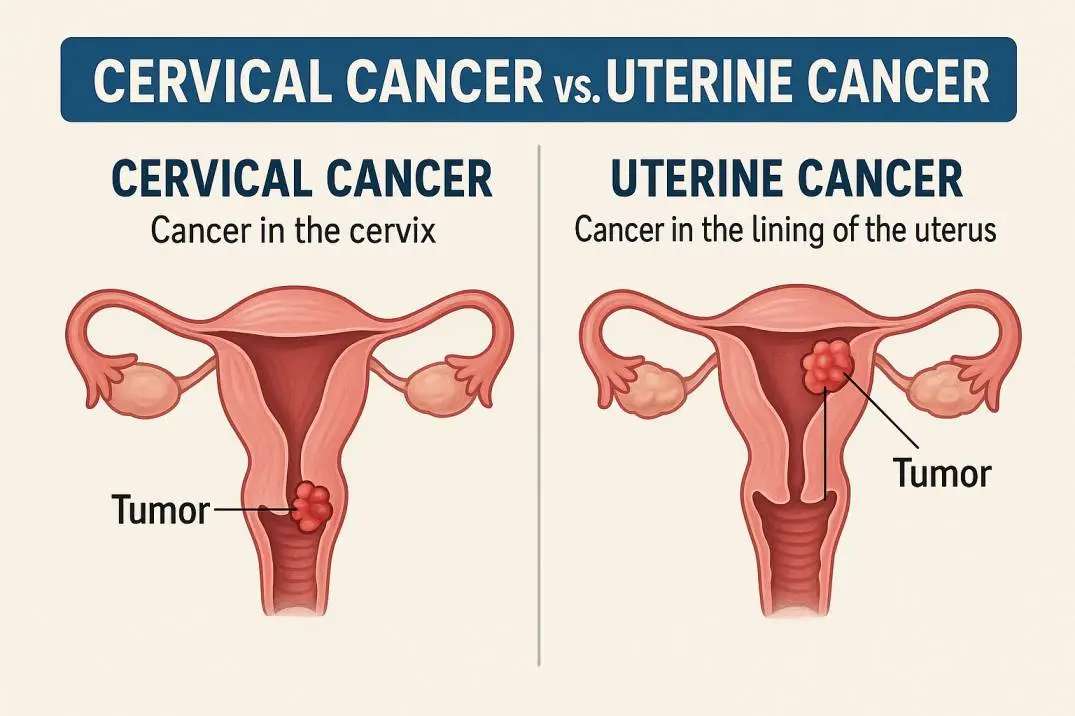
Uterine and Cervical Cancers
Uterine and cervical cancers are significant health challenges for women. Uterine cancer primarily impacts the uterine lining, while cervical cancer originates in the cervix, the lower section of the uterus. Regular screenings, such as Pap smears and HPV tests, are crucial for early detection. This significantly enhances treatment outcomes and survival rates.
Furthermore, ongoing research into targeted therapies and immunotherapy is advancing the management of these cancers. It offers hope for more effective and personalized treatment approaches.
Treating these cancers involves a strategic combination of surgery, radiation, and chemotherapy. This is tailored to the cancer's stage and type. For uterine cancer, treatment typically begins with a hysterectomy, potentially followed by radiation therapy to eliminate any remaining cancer cells. In contrast, managing cervical cancer may involve a loop electrosurgical excision procedure (LEEP) for early detection, followed by surgery or chemotherapy for more advanced stages.
Common Maternity Conditions
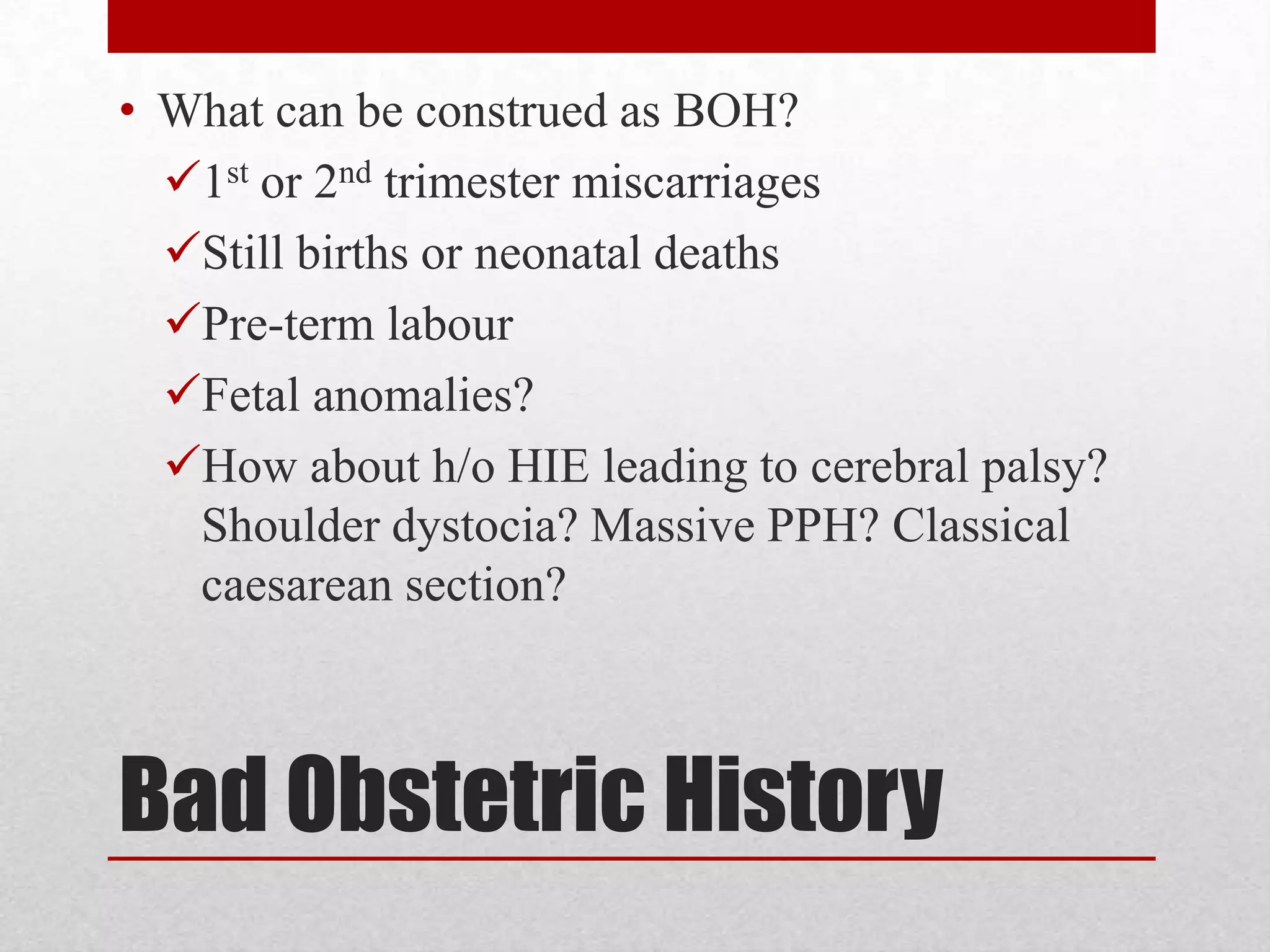
Bad Obstetric History (BOH)
Bad obstetric history (BOH) refers to a pattern of adverse pregnancy outcomes. These can include recurrent miscarriages, stillbirths, preterm births, or congenital anomalies. Causes can include genetic factors, uterine abnormalities, hormonal imbalances, infections, and conditions like diabetes or hypertension.
Managing BOH involves evaluating these causes through genetic counselling, hormonal treatments, or surgical interventions. Close monitoring and a multidisciplinary approach are essential to optimize outcomes in subsequent pregnancies.
Gestational Diabetes: A Common Concern
Gestational diabetes develops in about 6-9% of pregnant women. It occurs when the body cannot produce enough insulin to meet the heightened demands during pregnancy. Symptoms may be subtle but can include increased thirst and frequent urination.
To manage gestational diabetes, women are advised to make dietary adjustments, maintain regular physical activity, and monitor blood sugar levels. In some cases, insulin therapy may be required to ensure healthy blood sugar levels for both mother and baby. Research shows that managing blood sugar significantly reduces the risk of complications for both.
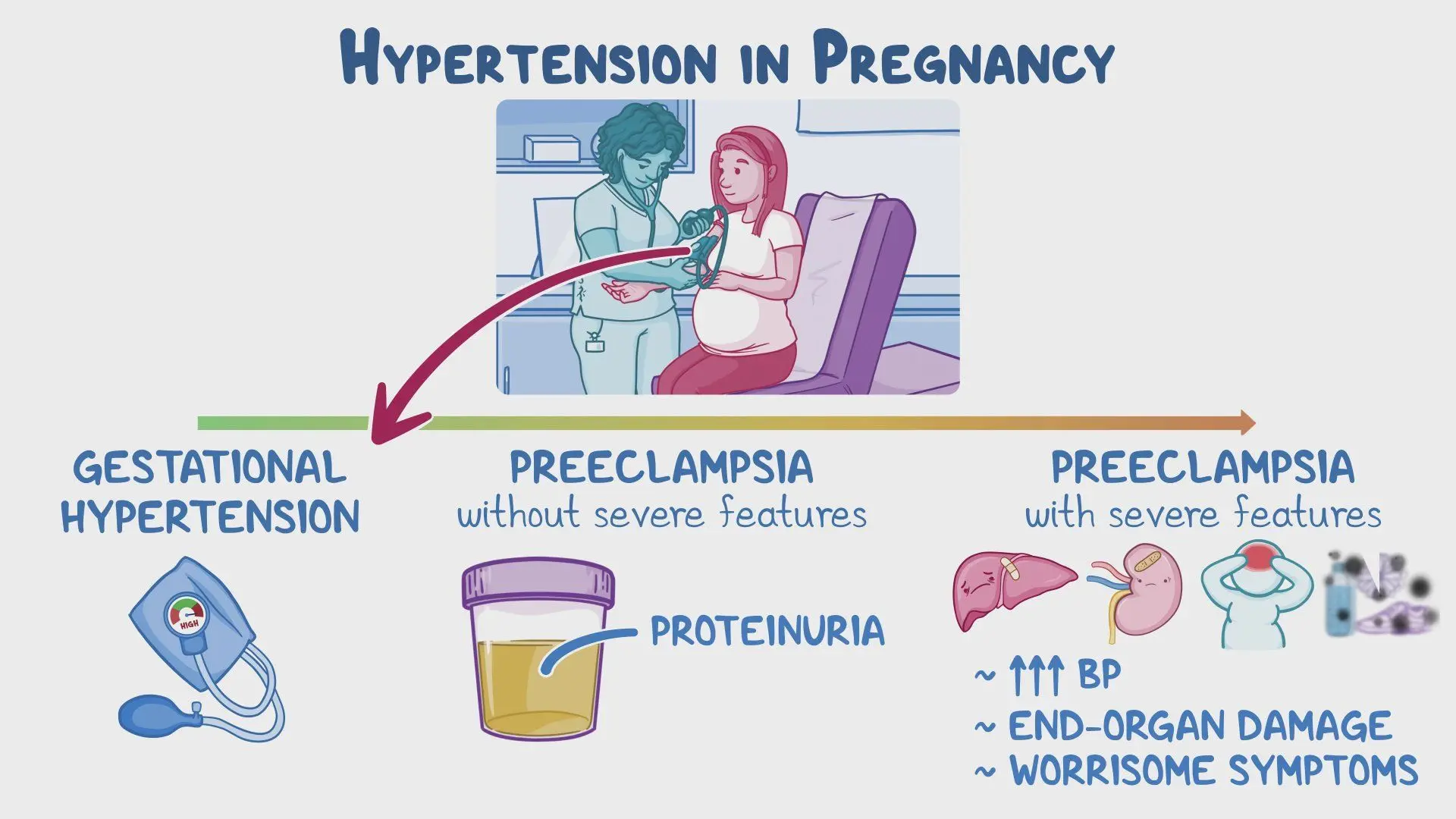
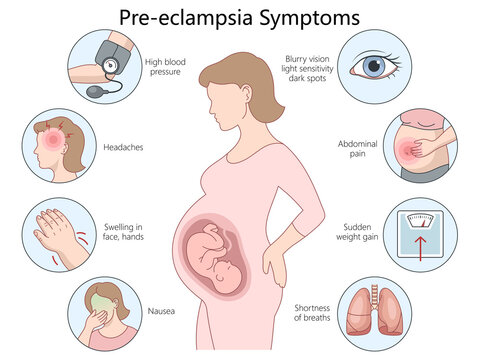
Preeclampsia: A Serious Condition
Preeclampsia is a serious pregnancy complication characterized by high blood pressure and signs of kidney damage. It affects about 5-8% of pregnancies. Common symptoms include swelling, sudden weight gain, and severe headaches.
The only definitive cure for preeclampsia is the delivery of the baby. Management usually involves closely monitoring the woman's blood pressure, using medications to lower it, and sometimes opting for early delivery if the condition worsens. Monitoring is vital; untreated preeclampsia can lead to serious health risks for both mother and child.
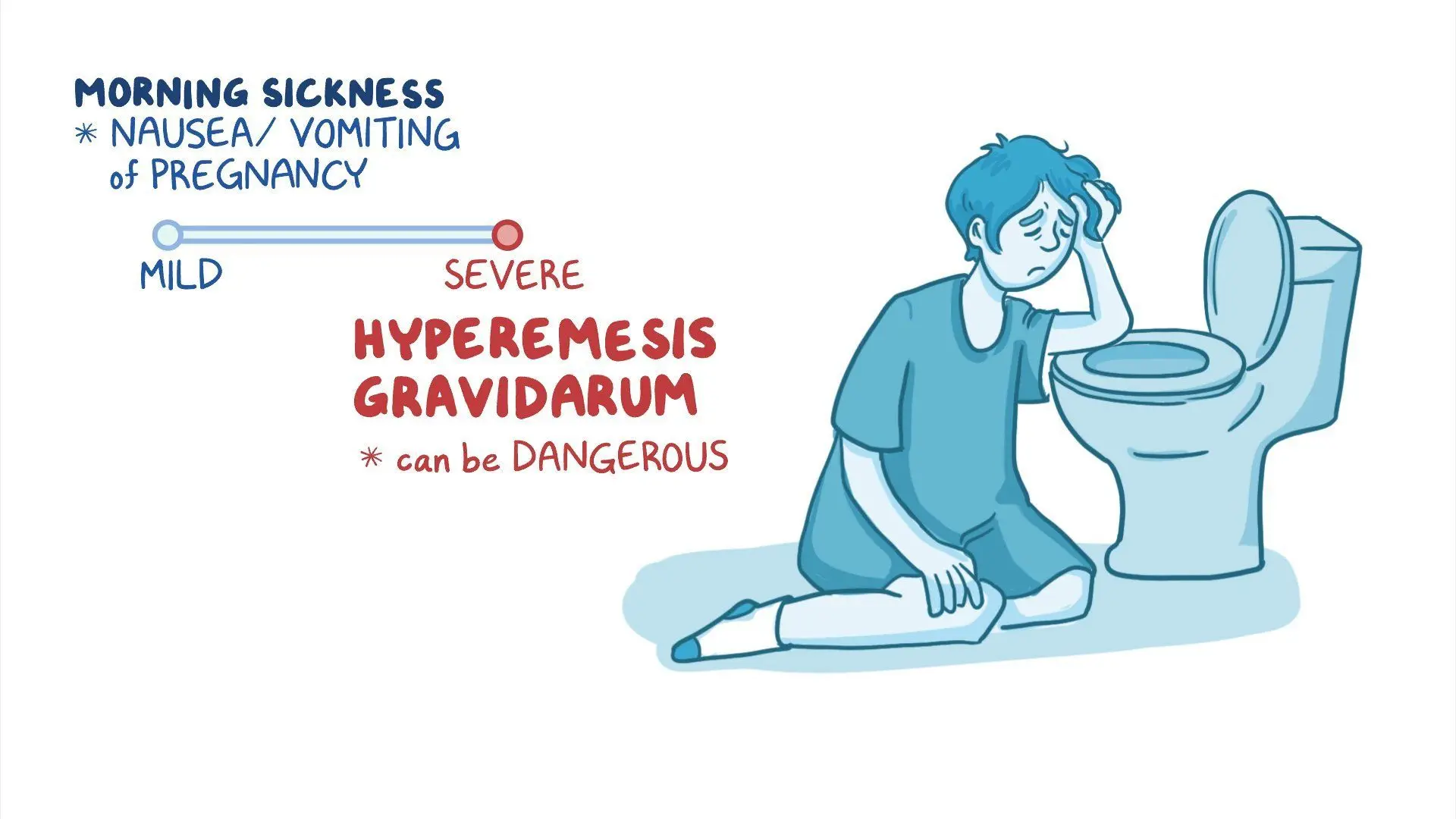
Hyperemesis Gravidarum: Severe Nausea
Hyperemesis gravidarum is a severe form of nausea and vomiting that affects around 0.5-2% of pregnant women. It can cause dehydration and weight loss, impacting daily life significantly more than common morning sickness.
Treatment often involves dietary changes, ensuring proper hydration, and medications to control nausea. In severe situations, hospitalization may be necessary for intravenous fluids and nutrition. Early intervention can help alleviate symptoms and improve overall quality of life during pregnancy.
Final Thoughts on Women’s Health
Understanding common gynaecological and maternity conditions is essential for women's health and well-being. By recognizing symptoms and seeking appropriate treatment, women can effectively manage these conditions. Regular check-ups with healthcare providers play a crucial role in early detection and intervention. This ensures healthier outcomes for mothers and their children.
Knowledge about health leads to better outcomes and an improved quality of life. If you or someone you know is experiencing symptoms related to gynaecological or maternity conditions, consulting a healthcare professional for guidance and support is vital.
For those seeking specialized care, I encourage you to consider a Gynaec & Maternity Consultation at Orchid Clinic, Akola.